Jacob Z. Hess, Ph.D.
Introduction. Since last summer, 5 students have taken their lives at one high school in Utah – leaving 5 families (and an entire school) blindsided, aching and searching for answers. That painful experience in one community is a microcosm of a broader state problem, which itself is a microcosm of a painful national problem.
Despite heroic efforts to reverse the trend, suicide is increasing everywhere – and for virtually every age level.[1] And that includes Utah. And that includes our youth.
But why? And why has the problem worsened in Utah over recent years – and among teens, in particular?
“We’re racking our brains,” said the principal of that high school in mourning. And as Stephen Eliason, a remarkable state legislator who has made this his cause, recently admitted, “Our children are dying….Apparently what we’re doing is not sufficient to save our children’s lives.”
So the obvious question on so many minds and hearts becomes this: What else more is needed?
Pursuing additional answers. How desperately so many want to answer that question – including me. Even the most passionate advocate, however, inescapably operates within the terms of the prevailing conversation we’re having about mental health. And I’m personally convinced that the nature of that (public and professional) conversation about both mental health and suicide continues to constrain in significant and serious ways what exactly we’re able to both see and do together. Bringing more attention to the terms of that conversation has been a central focus of my work for years (see these three essays, these two videos + this online class).
Conversation details aside, though, it’s crucial to acknowledge the degree to which people from a wide range of perspectives share a rock-solid commitment to finding more answers and solutions. Taking Utah as a case study, for instance, our good governor has convened an impressive task force of leaders working hard to make progress. The many other other counselors, educators, parents and doctors involved are all undoubtedly doing the best they can, based on what they know and the information they have available.
My purpose here is to share more information relevant to this discussion. We can, after all, only respond to what we know, and what we are aware of. In the spirit of a no-stones-unturned conversation with all views on the table, I raise another possible contributing factor that I believe needs to be taken more seriously. There are some in my field who would argue it’s an empirical reality – even an undeniable one.
Whatever the case, I write because this possibility is one we’re hardly even talking about it in Utah (or America at large, for that matter) – at least, not publicly and not in a way that reaches those families directly facing the realities of serious mental and emotional distress on a daily basis. I believe that needs to change – especially if this factor helps explain some of the troubling rise in American suicides, especially among youth.
In what follows, I will draw on statistics from my home state of Utah relative to pediatric antidepressant use to illustrate a pattern with applicability all across the United States. Along with a broader review of relevant literature in the area, I reached out while preparing this to some of the Utah leaders most involved in working to reduce youth suicide. Due to the sensitive (and, indeed, life-and-death) nature of this conversation, this material has been reviewed by multiple Ph.D. and M.D. colleagues whom I respect (including a number who are fond of disagreeing with me!) Although the material is substantial, my intent is to lay out the full picture of some details that arguably ought to play a much larger role in our ongoing public conversation about suicide. My hope is to reach those with a vested interest in this subject, enough so to spend the time it takes to seriously consider this additional data (with credit given to Dr. David Healy and Dr. Jonathan Leo, whose work I draw upon extensively here).
No matter what personal, professional, or philosophical view you bring to this issue, I plead with readers to keep an open mind to what follows. If nothing else, do it for the teens still, as yet, struggling mightily. Heaven knows, they deserve every bit of heart we can give to this conversation.
A humbling ache. Most people’s response to these rising suicides has been some form of deep humility and appropriate uncertainty, as school officials, government leaders, health professionals and especially parents, search for more answers.
This definitely makes sense, given how many complex variables can potentially contribute to any given suicide death. As Michael Friedrichs, a statistician working on the epidemiology of suicide in Utah, told me, “Everyone has their pet theory of the reason for the increase. There is no smoking gun.” Speaking of the Utah analyses he has been involved in, Friedrichs summarized elsewhere, “Our investigation showed that suicide is complex and youth can experience multiple risk and protective factors. No single behavior or risk factor could explain all the reasons for the increase we’ve seen.”
The broader research literature confirms this, with a Pubmed search of “suicide” and “risk factors” revealing well over 15,000 scholarly articles – and documenting a dizzying array of possible contributors. Factors commonly cited as making a likely contribution to increasing suicide rates among youth include a more pervasive social media and digital presence, wide-spread sleep deprivation and a nutrient-deficient American diet, growing cyber-bullying and social anxiety, the unsettling influence of compulsive pornography use, and the uniquely painful trauma of sexual abuse or assault. Underscoring perhaps the most important theme across studies, a 2014 Utah summary of factors involved in youth suicide notes that “Suicide is also often preceded by a lifetime history of traumatic events.”
The sheer complexity of research makes it clear that a starting point for any honest conversation about suicide has to be the overlapping interplay of many factors involved.
This is not a starting point always taken for granted by everyone, however.
‘No mystery for us.’ A subset of voices continues to insist that certain pathological factors unique to Utah culture are to blame for a recent increase in youth suicide. For instance, in an interview on a national news site, Troy William referenced the uncertainty of state officials pertaining to the rise in suicide as a stark contrast to his own confidence: “For us, there is no mystery to why young people are taking their lives in this state.”
He goes on to reference concerns with Latter-day Saint teachings that conflict with his own community’s sense of identity and self. No doubt, such a conflict can be an intensely existential and philosophical challenge for many teens (and adults), especially when vulnerable individuals are required to take up these personal and sensitive questions within an atmosphere of harshness, accusation and pressure.[2]
Given the unique increase in youth suicide within Utah, it’s also not hard to understand why some would wonder about a connection to the local conversation happening around gay rights (and the ongoing hesitancy from communities of faith). In the most recent CDC report breaking down the most immediate, local evidence, of the 40 cases including information on sexual orientation, only six (15%) were identified as sexual minorities however. While some teens, no doubt, kept that information hidden, it’s clear there is something else going on (and undoubtedly many things going on) beyond identity conflicts that help explain the recent increase.
Even so, some continue to insist that no other factor could account for the increase, arguing that this is the only shift that has occurred during this time period where suicide has increased in Utah.
But that’s simply not true. Alongside the many other factors cited earlier, there is another significant shift that has happened in Utah during this same period, centered on the one factor most widely known to directly influence mood: mental health treatment.
Another recent shift. During this same period of concern, something else happened in Utah: namely, a significant shift in the mental health conversation within the Latter-day Saint community centered in Utah and the surrounding regions. Although mental health had been addressed in many ways over the years within Latter-day Saint leadership, no senior apostle had addressed it directly since Elder Boyd K. Packer and Elder Bruce R. McConkie’s counsel years earlier. When Elder Jeffrey R. Holland took up the topic, he did so with characteristic force and power.[3]
And as most Latter-day Saints would agree, this talk had a profound impact – though, I have argued, not necessarily in the way I believe Elder Holland anticipated (or intended). In addition to drawing more attention to mental health issues generally, Elder Holland’s talk has been interpreted by many as direct encouragement for struggling Latter-day Saints seek medical support for mental health challenges – with some people taking away the message that psychiatric management was even something that God “expects us to use” (selectively citing four words from his talk).
Note to fellow Latter-day Saints: It would be inaccurate to characterize what follows as some kind of an “attack” on the Church. I’m arguing here that we have taken words from Elder Holland – a leader I love and respect – and over-interpreted them to our detriment. I am a defender of the faith, not an accuser…which is precisely why I’m writing this! From the research I’ve reviewed and completed myself, I cannot help but see under-acknowledged patterns that pose a significant threat to our Latter-day Saint teens (and any teen, for that matter). So with as much sensitivity as possible, I’m raising the concern here. If we are to make any progress on the serious matters in front of us as a society, I’m among those convinced that we must get better at having hard (but productive) conversations about our disagreements…including within different faith communities.
If my precious faith community is nothing else, we are a group of people trying to be obedient to our dear prophet leaders – even when they counsel us to do something that may seem scary. And while American adults are generally reluctant to take any kind of medication (especially long-term), surveys have documented a particular reluctance around psychiatric medication (especially when it comes to children and adolescents). That’s generally not something parents want to do. And that natural resistance partly explains why I believe Elder Holland’s talk was so impactful.
I once spoke to a couple who felt deep resistance to putting their son on a psychiatric medication for certain emotions and behaviors he was struggling with. But when their doctor pressed them to consider it, they overrode their internal hesitancy and did what he asked. I believe that for many families hesitant about turning to medical intervention, Elder Holland’s talk was enough to persuade them to overcome (or override) this resistance. For this reason, it should not surprise anyone if between 2013 and today (compared to the period of time prior to this talk), many more Latter-day Saint families (maybe in the order of tens of thousands) have sought out and accepted medical treatment for whatever depression, anxiety or other mental health challenges they face as a family.[4]
For all these reasons, I do not think it overstates the case to suggest that this talk accelerated an (already ongoing) sea-change in Latter-day Saint mental health attitudes, especially in regards to medical treatment. Indeed, a series of videos in an associated LDS mental health campaign has had viral viewership.
Expanding treatment as an unmitigated good? As you would expect, this shift has widely been hailed among medical professionals as an undoubtedly positive step. For many involved in the conversation, it’s taken for granted that if more people get help, then less people will be suffering…which only makes sense, right?
Although in general terms that’s certainly the truth, the particulars matter here. And while it’s true that most interventions produce some kind of immediate benefit, this simply cannot be said when it comes to the long-term outcome trajectories associated with all available treatments.
In an article Jeff Lacasse and I wrote several years ago about youth mental health, we argued for an urgency to go beyond a simplistic treatment debate about “what works” – to look more carefully at what it means for something to “work” or be “effective” or “successful.” And if, by “successful,” we mean long-term success, it’s simply not possible in an honest conversation to see all treatments as equally “successful.” As I detailed in another recent review, whatever initial benefits people may legitimately receive with antidepressant treatment, much of the available evidence confirms that outcomes associated with longer-term use are troubling, at best.
Indeed, rather than seeing what one would expect with increasing treatment rates (aka, decreasing rates of mental/emotional burden), the rates of mental disability across the Western world have expanded sharply since the widespread implementation of antidepressants as a first-line treatment.
Over the long-term, suicide rates have also grown to record levels in many of these same countries. If that is true throughout many different countries, should it surprise us to see similar increases taking place in Utah in the last decade as we have come to increasingly conform to the same approach to mental health management as the rest of the country?
WARNING: People who have been prescribed antidepressants should not suddenly stop taking their medication. Anyone considering altering the dosage of their medication, or withdrawing from it, needs to consult with professional support you trust to help you navigate the details. Withdrawal from psychiatric drugs should be done cautiously with professional supervision.
Four different American “sea changes” in attitudes towards antidepressant use for children. The existence of distinct time-points where there have been discernible “sea changes” in attitudes towards youth treatment seems clear in the historical timeline. Noting some of these same shifts, Dr. Jonathan Leo wrote in 2006, “Ten years ago, the market for antidepressants in children was practically nonexistent, 5 years ago it was booming, and now [shortly after the U.S. “black box warning” was added to antidepressant packaging], it seems to be in jeopardy.”
I believe these different shifts provide compelling data-points from which to derive important clues for what is going on. The specific attitudinal shifts that I would propose for consideration include three national shifts and the fourth Utah-specific shift noted above:
- (1) From 1997 to 2003, youth prescription rates for antidepressants rise sharply following the publication of a single study by Graham Emslie and colleagues which reassured parents that Prozac was “safe and effective” for youth.[5]
- (2) From 2003 to 2007, youth prescription rates for antidepressants drop following FDA health advisories and warnings that cautioned Americans about a heightened risk of suicide with antidepressant treatment for youth.
- (3) From 2007 to 2013, youth prescription rates rise once again as widely publicized, compelling critiques of the black box warning persuade many physicians and parents to essentially ignore the cautions.
- (4) From 2013 on (in Utah, Idaho and other Latter-day Saint gathering places, in particular), youth prescription rates almost certainly increase following the general conference message noted above.
Reviewing Utah-specific suicide statistics for teens during this period, it’s hard not to notice shifting trends that correspond to each of these periods:
- (1) From 1997 to 2003, a noticeable and significant increase in youth suicide numbers.
- (2) From 2003 to 2007, a noticeable and significant decrease in youth suicide numbers (peaking in 2003/2004, then decreasing).
- (3) From 2007 to 2013, a noticeable and significant increase, once again, in youth suicide numbers.
- (4) Since 2013, a noticeable, and significant jump in these same numbers.

More than simply a rise in completed suicides starting in 2013, it’s important to note how all relevant statistics for youth suicide risk rose significantly between 2013 and 2015. A 2015 Utah Prevention Needs Assessment sponsored by the Utah Department of Health, Bureau of Health Promotion found that in 2015:
- 24.8% of Utah students reported they felt sad or hopeless (compared to 20.8% in 2013)
- 16.6% reported they seriously considered attempting suicide (compared to 14.1% in 2013)
- 13.5% reported they made a suicide plan (compared to 10.8% in 2013)
- 7.6% reported they attempted suicide one or more time (compared to 6.2% in 2013).
I am raising the possibility here that one common thread across all these different shifting trends is the corresponding shift in parental and professional attitudes toward mental health treatment in different periods of time. I offer this as a plausible explanation for the shifting suicide rates, due to its direct tie to the most proximal variable associated with intentionally changing youth mood – namely, psychotropic medications.
To be clear, no one is arguing that medical intervention increases the suicide risk for everyone. That would be an absurd argument, given the benefit many have experienced with antidepressant treatment. The question is understanding accurately how many for whom there is a legitimate risk of increased suicidality and how to determine whether that risk (for those people) is worth taking for the benefits others are receiving. In order to answer that question adequately, however, we need to have a more rigorous conversation about what the best available research actually documents, free from industry influence.
Grappling with this possibility. Stay with me! Please don’t stop listening – even if it feels challenging. There is much more to say. For instance, if this claim is legitimate, it certainly deserves more than population-level observations to back it up (as I have made above, and as others have made to argue for an opposing view).
With little awareness of the patterns arising from controlled clinical studies, however, many people remain incredulous at the possibility of antidepressants prompting suicide risk. But in fairness, the idea that increased antidepressant use can be associated with a heightened suicide risk is not some new-fangled “theory” being promoted. It’s on the package of every anti-depressant!!


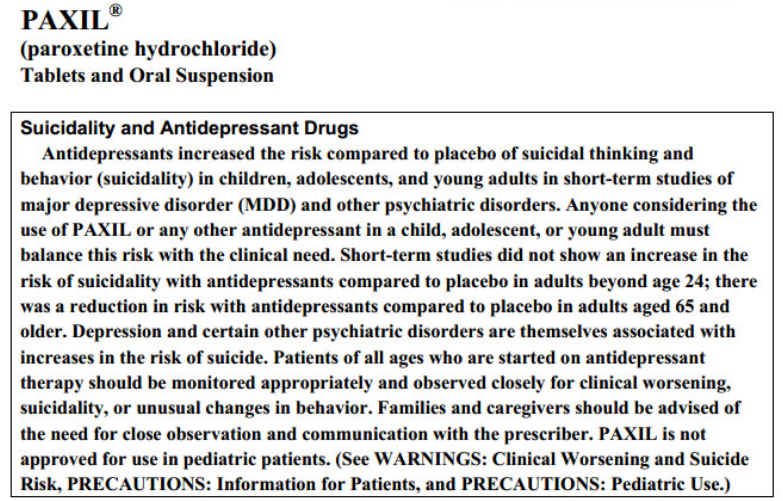
Ever since the FDA issued a black box warning for antidepressants in 2004, this message has been mandated by law to be on the packaging (See here for examples of all SSRI black box warnings for child suicide).
How and why this warning came about, however, and whether it was ultimately a good thing has subsequently been sharply contested.
REMINDERS: Anyone experiencing suicidal thoughts is asked to call the 24-Hour National Suicide Prevention Hotline, 1-800-273-TALK (8255). Utah also has crisis lines statewide, and the SafeUT app offers immediate crisis intervention services for youths and a confidential tip program.
If someone you know exhibits warning signs of suicide:
- Do not leave the person alone
- Remove any firearms, alcohol, drugs or sharp objects that could be used in a suicide attempt
- Call the U.S. National Suicide Prevention Lifeline at 800-273-TALK (8255)
- Take the person to an emergency room or seek help from a mental health professional
Warning about the black-box warning. When the SSRIs first came on the market in the late 1980’s there were hints of increased suicidality in people (mostly adults at that time) taking the drugs.[6] This admission began showing up in academic journals by the early 1990’s. For instance, the possibility of antidepressants inadvertently leading to “the promotion of suicidal thoughts and behavior” was acknowledged in a 1990 Lancet Editorial. And several published studies at the time noted uncharacteristic self-aggression that began after patients started antidepressant treatment, and which then abated when patients discontinued treatment:
- Teicher MH, Glod C, Cole JO. (1990). Emergence of intense suicidal preoccupation during fluoxetine treatment. American Journal of Psychiatry;147: 207-10. [“Six depressed patients free of recent serious suicidal ideation developed intense, violent suicidal preoccupation after 2-7 weeks of fluoxetine treatment. This state persisted for as little as 3 days to as long as 3 months after discontinuation of fluoxetine. None of these patients had ever experienced a similar state during treatment with any other psychotropic drug.”]
- King A, Riddle MA, Chappell PB, et al. (1991). Emergence of self-destructive phenomena in children and adolescents during fluoxetine treatment. Journal of the American Academy of Child and Adolescent Psychiatry;30:171–176. [“Self-injurious ideation or behavior appeared de novo or intensified during fluoxetine (Prozac) treatment.”]
- Rothschild AJ, Locke CA.(1991). Reexposure to fluoxetine after serious suicide attempts by three patients: the role of akathisia. Journal of Clinical Psychiatry;52: 491-3. [“Three patients developed severe akathisia during retreatment with fluoxetine and stated that the development of the akathisia made them feel suicidal and that it had precipitated their prior suicide attempts. The akathisia and suicidal thinking abated upon the discontinuation of the fluoxetine”].
- Masand P, Gupta S, Dewan M.(1991). Suicidal ideation related to fluoxetine treatment. New England Journal of Medicine, 324: 420.
In light of this evidence, the first FDA committee convened in 1991 to consider taking action on a warning specific to Prozac. Especially given the ethical requirement of informed consent, this seemed to be a sensible, and even urgent precaution to make. At this early FDA hearing, testimonies from a number of families who had lost loved-ones were heard, speaking of self-harm “totally out of character” for people.
Despite these early indicators, the FDA committee voted against a formal warning. The head of the FDA’s Division of Neuropharmacological Drug Products at the time, Dr. Paul Leber, argued that the only assessments “deemed reliable in the scientific community” (randomized controlled trials at the time) “did not indicate any risk of suicidal thoughts, acts or behaviors” – effectively, in the words of one journalist, “dismiss[ing] all of the anecdotal testimony with one sweep of his tongue.” [7]
Another argument made at the time was that such a warning might scare people away from treatment. Dr. Leber argued that if a stronger precaution was put on the label, “the result might cause overall injury to public health.”
What kind of an injury?
Undertreatment as the central problem. Scientists at the hearing speaking on behalf of pharmaceutical companies emphasized what they characterized as a stark undertreatment of depression that they argued played a central role in suicide incidence. Gary Tollerson, an Eli Lilly scientist, said “it is our feeling that the major public health concern relative to suicidality and depression is the current stigma, under-recognition and undertreatment of a very serious disease.”[8]
That argument initially underscored by company spokespersons continues to be shared widely today. For instance, the director of Utah’s Chapter of NAMI said in 2007, “We have to acknowledge the elephant in the room” – going on to argue that the leading cause of suicide was, once again, “untreated or undertreated mental illness.”
The painful reality, of course, is that many youth and adults who end up taking their lives have been in treatment. In an analysis of “precipitating circumstances for [teenage] suicide decedents” in Utah, it was found that “of those with diagnosed mental health problems, 84% were noted to be receiving mental health treatment at the time of death” (Utah Health Status Update – CDC Investigation Shows Youth Suicides in Utah Increasing, Dec 2017). One teenage boy struggling with depression told a Hope Squad leader at his local high school that he didn’t want to go on antidepressants since his friend who took his life had been on them.
As I will explain later on, there are a number of reasons why this disconnect doesn’t seem to register or cause alarm in public discussions about suicide, one of which is that our focus is fixed in an entirely different direction. Indeed, as reflected above, rather than exploring other support options in light of documented concerns with current treatment approaches, in many ways we have been persuaded that our great need is getting more of the same treatment to even more people.
Is this a wise course of action in light of the available evidence?
Prevailing assumptions about mental health treatment. This has been an almost unquestioned assumption guiding public mental health policy over recent decades. Over the last three decades, in particular, enormous resources have been expended to make sure more people get access to treatment. In Utah, for instance, there have been almost ceaseless efforts to widen treatment access, from extensive initiatives to screen kids for mental illness in the juvenile justice and foster care systems, to increasing opportunities for the uninsured to receive treatment, to expanding the number of touch-points between youth and crisis counselors or crisis hotlines.
Even amidst the suicide spike in Utah, it continues to be almost universally taken for granted that the indispensable task remains “how to successfully find and treat suicidal kids” – with prominent leaders continuing to call for additional steps in reaching people sooner and earlier in order to get them services and treatment (e.g., “How to curb Utah’s teen-suicide rate? Hatch-convened roundtable says kids needs access to mental-health services”).
No doubt, it is a good thing to make sure people have support, help and someone to talk with. Isolation is good for no one – and breaking out of that is crucial. No one disagrees on that point.
But when they do talk with someone, what are they hearing? And what are they being encouraged to do (or not do) to get additional help? It goes without saying that medical outreach has become central to almost all mental health intervention in America today. In one recent mental health training to leaders attended by my colleague in his faith community, there was encouragement to make sure anyone exhibiting signs of mental health distress was immediately encouraged to go to a doctor. And in a report about Utah’s ongoing discussions about suicide, a local health care administrator spoke about working on “plans to address it at the level of primary care.”
To be clear: Doctors have an important place in this conversation, and one that should be respected. I believe they can be an important part of this solution. What I’m pointing out here is that a central and overriding focus in recent decades of suicide prevention has been increasing people’s willingness to reach out to doctors and to be willing to accept treatment.
A rapid expansion of medical treatment for mental health problems. Thanks to similarly focused efforts like this all across the country, treatment has indeed increased all across the United States at a remarkable pace. For instance, a 2011 report released by the National Center for Health Statistics (NCHS) showed that the rate of antidepressant use in this country among teens and adults (people ages 12 and older) had increased by almost 400% between 1988–1994 and 2005–2008 – leading to estimates of one in every 10 Americans taking an antidepressant.[9] A 2013 report likewise found approximately one in six U.S. adults reported taking a psychiatric drug, such as an antidepressant or a sedative.[10] And a 2006 review found 12 percent of adults reporting that they were on an antidepressant,[11] with SSRIs the third most prescribed drug in America since 2005.[12]
As Bob Whitaker and others have been pointing out for the last decade, however, despite these kinds of dramatic increases in antidepressant use, there is a great deal of evidence that the burden of mental/emotional distress has worsened and increased during this same time period. That’s just the truth.
Interestingly enough, however, the opposite argument has been made for years when it comes to suicide rates: that the introduction of antidepressants in a country has corresponded to a decrease in suicide over time. In a 2008 commentary on population-level correlation studies from which these arguments are derived, Reseland and colleagues note that “such studies have led to claims that antidepressant usage has brought about falls in suicide rates in Sweden, in the United States, in Australia, in Finland, and more generally in all countries where antidepressant use has increased.”
These population-level correlation studies have frequently been cited as a strong rationale for why (a) concerns about an antidepressant-suicide connection are inflated, and overstated and (b) our real concern should, once again, be making sure more people are encouraged to embrace antidepressants as part of reducing their suicide risk.[13]
Inescapable confounds for population level correlations. Despite their impressive scope and sweeping claims, researchers are well-aware that population-level correlations involve complexities not possible to account for or control, with several fundamental challenges in their design and interpretation.[14]
At times, a correlation arising from these kinds of studies can be so compelling that much less attention goes to the details of how it is generated. Specific to this “more antidepressants => less suicide correlation,” for instance, Dr. Marc Stone raised concerns about the “identification of trends or changes in what could well be random fluctuations,” citing specific examples of “framing of ‘before’ and ‘after’ periods that absorb changes or trends that may have begun either well before or well after the issuing of the boxed warning (or some other dividing point), or use of inferior data sources when better sources were available.”
Perhaps due to the many variables potentially influencing population-level correlations, they have been used in suspect ways over time, to reach many eye-catching, but dubious conclusions, including arguments (a) that pornography use decreases rape in society and (b) that youth suicide rates are connected to the specific concentration of Latter-day Saints in a particular location.
Given their wide flexibility, these kinds of methodologies have been undeniably convenient to different corporate interests in the past. For instance, Dr. Healy points out that in the 1960’s, “tobacco companies denied there was a link between smoking and either lung cancer or cardiac disorders on the basis of 60 years’ worth of national data showing falling deaths from respiratory and cardiac causes and increased life expectancy coincident with increased cigarette consumption.”
To be clear, these same limitations apply to all comparable analyses, including correlations between increasing antidepressant use and long-term trends of government disability pay-outs due to mood disorders.[15]
The reality, as noted earlier, is this: these are complicated questions that not easy to navigate. While these general correlation methods provide interesting arguments worth exploring, on their own, they simply cannot establish the truth of the matter. As Dr. Healy states, “While it may seem hard to disentangle the role of these two variables, the disease and the drug, there is a way, and it has been done. The place to begin is with the companies’ own efficacy studies.”
That’s where we will go next.
Clinical study results: Antidepressants double suicide risk for teens. After the FDA’s initial rejection of a warning label, subsequent analyses were supplemented by reviews of more controlled clinical outcome data that eventually persuaded the agency to act. The pediatric meta-analysis data on which the FDA deliberated in 2003-2004 are written up in detail (all 131 pages here), and published formally by Hammad and colleagues in 2006.[16] In lay language, the individuals in the studies who took the drug were about twice as likely to have been actively thinking about suicide, made a suicide attempt, or made preparations to die by suicide, when compared to those receiving a placebo.
As this research team went on to state, “the observed signal of risk for suicidality represents a consistent finding across trials,” summarizing the takeaway as follows: “when considering 100 treated patients, we might expect 1 to 3 patients to have an increase in suicidality beyond the risk that occurs with depression itself owing to short-term treatment with an antidepressant.”[17]
Corroborating evidence from overseas reviews of the same data were also released at this time. This included data from a review of suicidal behaviors posted by British regulators in 2004 showing a 2.62-fold increase in completed suicides and a 2.4-fold increased risk in suicides and suicidal acts for youth taking antidepressants, compared with placebo (see Tables 1 and 2 for raw numbers).[18]
Despite this, some confusion remained due to the conflicting claims cited above, leading to a confusion where data seemed to suggest divergent conclusions about antidepressants and suicide risk. For instance, Healy pointed out in 2003, “Meta-analyses of RCTs conducted around this time indicated that SSRIs may reduce suicidal ideation in some patients. These same RCTs, however, revealed an excess of suicidal acts on active treatments compared with placebo.”[19]
In response, one research team in 2005 sought to do a comprehensive review of 702 studies submitted to government regulators on suicide risk (totaling close to 87,650 patients studied). The key finding from this exhaustive review by Fergusson and colleagues was a significant (more than twofold) increase in the odds of suicide attempts for patients receiving SSRIs compared with placebo or other interventions.
The following year, a research team lead by Dr. Olfson in the Department of Psychiatry at Columbia University compared Medicaid beneficiaries across the country who had similar patient profiles, except for differences in whether they received antidepressant treatment or not. While noting no significant difference in adult suicide attempts or death, they noted, “In children and adolescents (aged 6-18 years), antidepressant drug treatment was significantly associated with suicide attempts and suicide deaths.”[20]
Two other observational studies that followed are worth mentioning:
- Umetsu and colleagues reported in 2015 on a large epidemiological study based on data from the Food and Drug Administration (FDA) Adverse Event Reporting System database, with analyses indicating associations between SSRI treatment and suicidal and self-harm events. As with other studies, these associations were stronger in the under 18 group than other age groups.
- In a 2016 observational study of 392,458 Denmark medical records, Christiansen and colleagues found “a significant overlap between redeeming a prescription on SSRIs and subsequent suicide attempt.” They found, specifically, that “the risk for suicide attempt was highest in the first 3 months after redeeming the first prescription.”
Finally, in a more recent 2016 review, a research team in Denmark analyzed data from 70 trials (64381 pages of clinical study reports) involving 18526 patients submitted to European and UK regulators. Similar to other studies, they found a doubling of the risk of suicidality for children and adolescents taking antidepressants.
In light of so many clinical studies documenting a doubling of suicidality in youth, Dr. Healy states the obvious: “This is not an isolated finding, but is the case for almost every single antidepressant studied.” He adds, “No longer can we simply blame the disease: the drugs appear to be playing a role in making some people more likely to take their lives.”
To be clear, no one is arguing these kinds of risks show up for everyone taking these medications. The concern is the percentage of youth where this does happen – and what this means for our widening use of these medications on a mass scale. Dr. Phillip Hickey summarizes:
No one on this side of the issue is suggesting that a large proportion of people taking antidepressant drugs kill themselves….What is being contended, however, is that these drugs are inducing strong suicidal urges in a relatively small proportion of individuals who had not previously had thoughts of this kind, and that some of these people are succumbing to these urges, and are taking their own lives. This is … very important, and it warrants investigation even if it involves only a fraction of one percent of the people taking the drugs. To dismiss these widespread and credible contentions on the basis of the dogmatic insistence that the drugs are wholesome, or that the individuals were probably suicidal to begin with, is simply unconscionable.
Despite this extensive evidence pointing to a significant concern, it’s remarkable to see how much minimization, denial and dismissal continues to happen in our current mental health conversation. Admittedly, some of that questioning happens due to understandable confusion at the level of individual cases.
Is it me or my med? In fairness, how exactly to interpret a mixture of effects arising internally is not always easy, as demonstrated in sociological studies such as David Karp’s text, “Is it Me or My Meds?” I saw this same confusion in my own study of people on antidepressants, including one woman who experienced panic attacks for the first time after starting an antidepressant, and grappled to know whether that was drug-induced or a manifestation of an underlying anxiety problem she had not recognized.
That’s not always (and not usually) an easy determination to make: What is coming from the drug versus the disorder? Rather than acknowledging the complexity and case-by-case variability to this question, an interesting and remarkably definitive pattern of interpretation has emerged:
- When positive thoughts, feelings and experiences arise for someone taking an antidepressant, they are (generally speaking) attributed to the medication.
- When negative thoughts, feelings and experiences arise for someone taking an antidepressant, they are (generally speaking) attributed to underlying disorder.
In this way, when a suicide happens, we are almost primed as a society to see that arising from underlying mental illness, rather interventions attempting to treat that illness. Given the obvious connection between psychological distress and suicide, Dr. Healy notes that “naturally, to accusations that the drugs cause some people to take their own lives, the companies’ response has always been: It’s the disease, not the drug.”
In some cases, however, the direct evidence of a given case seems to confirm that someone wouldn’t have done this without the drug.
The evidence of uncharacteristic behavior. Referring to the FDA analysis prior to the black box warning, Dr. Newman, a member of the Psychopharmacologic Drugs and Pediatric Advisory Committee that helped review evidence of suicide in youth, noted that it was persuasive to observe that “several of these cases involved patients who had shown no hint of suicidality before beginning treatment with the drugs and who had been given these drugs for indications other than depression, including migraine headaches, nail biting, anxiety, and insomnia.”
It was specific anecdotes like this that prompted well-respected researcher Martin Teicher to publish his early case studies in 1990 and 1993, including one young girl who, “began cutting herself after taking a high dose of Prozac – incessant self-mutilation.” The report goes on to note, “After this patient tapered off Prozac, her self-destructive behavior and suicidal thoughts disappeared.” Dr. Teicher added, “the reason why I believed that we were dealing with a drug-emergent effect is because the symptomatology that [patients] developed during the time they were on fluoxetine was unlike anything they had experienced prior to or following” [emphasis my own].
One father describes his experience, “In 2009 my son, who had never been depressed in his life, went to see a doctor over insomnia caused by temporary work-related stress. He was prescribed Citalopram, and within days he had taken his life. At my son’s inquest, the coroner rejected a suicide verdict, but delivered a narrative judgment, citing Citalopram by name as the ‘possible cause.’”
Rather than an anecdote or two, literally thousands of cases have been gathered with similar patterns (see these two online databases, here and here). It’s important to note that these adverse effect are not limited to youth facing depression, and indeed, often arise in youth who otherwise wouldn’t be expected to be suicidal (see Goodman 2006). For instance, Christiansen and colleagues documented in 2016 an increasing suicidality in low risk youth.
These would be important questions to ask any family who has suffered the loss of a child by suicide:
- Did your son or daughter start, end, or change the dosage of a course of antidepressants in the weeks leading up to this tragedy?
- If so, did you notice any other uncharacteristic behavior at the time?
For any family whose child is currently taking antidepressants, it’s also important to pay particular attention to dosage changes, and any uncharacteristic behavior. Rather than watching out for random shifts, it can be helpful to understand some of the unintended effects that are well-established in the clinical and research literatures. In what follows, we review three specific effects that have been known to occur with both youth and adults.
Patterns in adverse effects some experience. Let’s talk about what we know about the uniquely intense side effects some youth (and adults) experience at different times, particularly in the early weeks of uptake or if the dosage is increased, decreased, withdrawn, or changed for another prescription. [Evidence with youth is highlighted below – with citations of adult evidence provided in some cases].
One preliminary note to those who may be surprised by what follows. One of my colleagues at Colorado State, Shannon Hughes, focuses her research on the different ways that side-effects are narrated and framed. It shouldn’t surprise us, perhaps, that industry generated lists of side-effects look quite a bit different than patient reports. To get an accurate sense of what’s happening, it’s important to get a wide sense of what patients are actually experiencing and reporting.
Below we review three effects that have particular relevance for understanding on a more granular level why some people may experience a heightened risk of suicide while taking antidepressants.
1. Akathisia. This language shows up in the patent for Prozac, “akathisia (inner restlessness), suicidal thoughts, and self-mutilation,” labeled as “one of its more significant side effects.” Listen to how neuro-psychologist Dennis Staker describes his own drug-induced akathisia for two days: “It was the worst feeling I have ever had in my entire life. I wouldn’t wish it on my worst enemy.”
Another individual characterized it as “ach[ing] with restlessness, so you feel you have to walk, to pace. And then as soon as you start pacing, the opposite occurs to you; you must sit and rest. Back and forth, up and down you go … you cannot get relief.”
2. Amotivation/Apathy. In what they refer to as an “amotivational syndrome” associated with the frontal lobe, Dr. Jane Garland and colleagues report on five cases of youth prescribed antidepressants who came to experience a unique level of apathy and lack of motivation, sometimes accompanied by disinhibition. In each case, these symptoms were linked directly to dosage and were reversible after tapering back the child. But given (a) the similarity to depression’s own symptoms, (b) a child’s lack of insight in appreciating this and (c) the fact that the onset of this lack of motivation comes later on in treatment, Dr. Garland warns doctors about the strong likelihood of missing this possibility, and the need to carefully monitor children.
This phenomenon has also been studied and documented over the years in adult on antidepressants as well.[21]
3. Hyper-Activation/Disinhibition. Compared to the decreasing motivation just described, a seemingly opposite effect has been noted in research for years and acknowledged by the FDA as early as 2004 (see FDA report here). In 2003, Faeda and colleagues wrote about “treatment-emergent mania (TEM) or increased mood-cycling following pharmacological treatment” in youth, a subset of which experience “prominent suicidal behavior.” In 2006, Goodman and colleagues investigated one of the mechanisms behind suicidal behavior leading to the black box warning, noting that “during the course of SSRI treatment, some children may experience an ‘activation syndrome’ characterized by agitation, insomnia, irritability, brittle mood, and other signs of hyperarousal that, if unrecognized, could conceivably foster suicidality.”
Dr. Shauna Reinblatt and colleagues summarized their data in 2009 documenting the frequency of this “activation” involving specifically impulsivity, insomnia, or disinhibition. Compared to 23 youth in the placebo group (where 1 experienced these symptoms of restlessness), 10 of the 22 youth in the treatment group did (45%). Other studies have found between 10 and 50% of kids experiencing these same “activation” symptoms. On average, these symptoms emerged anywhere between week 1 and week 8 (with week 4 being the average).
Whereas some have attributed these manic episodes to a latent bipolar disorder (per our earlier discussion), other case studies confirm the frequency of this occurring as a drug-induced effect. For instance, Dr. Aggarwal reported in 2011 on a boy (without any present risk factors for bipolar patterns) who experienced “increased psychomotor activity, euphoric affect, racing thoughts, grandiose ideas, and inflated self-esteem” upon starting an antidepressant. Once the prescription was ended, these symptoms went away.
Despite this, physicians face a similar confusion as patients, at times, in determining how to assess what they are seeing (for instance, see this new article, “Primary Care Practitioners May Mistake Irritability as Bipolar Disorder in Youth“).
In summarizing the available evidence, Dr. Maya Amitai and colleagues wrote in 2015, “There is a clear and considerable risk of excessive arousal or activation, and even hypomania or mania, in children and adolescents treated with SSRIs. The rates of these symptoms, even those diagnosed as mania or hypomania, are much higher than in adults with anxiety and depression.”
In theorizing about the reason for the higher rates of hyper-arousal in children taking SSRI’s, Drs. Safer and Zito wrote in 2016, “Children are particularly vulnerable to specific [adverse effects] from certain medications, such as SSRIs. It is likely that the level of children’s biological immaturity explains part of this phenomenon.”
In light of both the clinical evidence and expanding reports from parents and professionals, the evidence became so overwhelming that the FDA eventually concluded in 2004 that a black-box warning on antidepressants was needed.
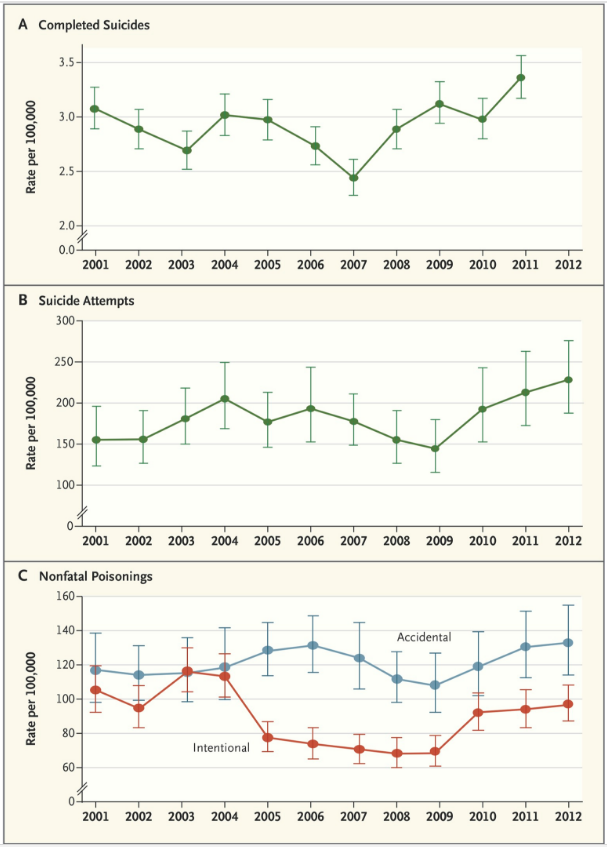
Black-box aftermath: Warnings about the warning. Following the warning issued by regulatory agencies in both the United States and Europe about possible suicide risk with antidepressant use in pediatric patients, SSRI prescriptions for children and adolescents decreased as expected. For instance, prescriptions for youths decreased by approximately 22% in both the United States and the Netherlands after the warnings were issued.
What happened next has been interpreted very differently. In a 2007 study, the authors argued that in the same period of decreasing antidepressant use among youth, there was a 14 percent increase in suicides in the United States, and a 49% increase in the Netherlands. Lu and colleagues also argued in 2014 that “there were simultaneous increases in suicide attempts among young people” in the period after the black box warning.
What more need be said? As soon as these papers came out, for many the case was closed. Remarkably absolute statements[22] connected to these claims were leveraged as a damning indictment of the black box warning all around the world.
Much less attention, once again, has gone to some of the details behind the claims.
Unfortunately, without this level of scrutiny, it becomes impossible to assess the true merit of these papers’ claims. I focus here on just three little-acknowledged problems with the data behind the claims just mentioned:
1. Inattention to the influence of plausible third variables. After acknowledging that “Most depressed persons who eventually commit suicide seek professional help within 1 month before death,” Dr. Gibbons and colleagues underscore their concern that “most are not on antidepressant medication at the time of death” and that “SSRIs are rarely found to be present at the time of death in suicide victims.”
This pattern, which has also come up in the Utah discussion on youth suicide, has been referenced as persuasive evidence behind minimizing the risk, including “suggest[ing] that lack of treatment contributes to suicide risk and that more widespread antidepressant treatment might reduce suicide rates” and that “SSRIs are not likely to be a causal factor in a substantial proportion of child and adolescent suicides.”
This begs the question, however, why were those who died by suicide not actively taking medication at the time? In addition to perhaps inadequate treatment management efforts, it’s common to hear mention of stigma, noncompliance and people’s hesitance to accept treatment. Virtually no comparable attention has gone to adverse effects some experience on the medication (leading many to want to stop) and to the common physiological and psychological turbulence that frequently arise anytime antidepressants are increased or decreased.
That this turbulence is not even mentioned in these studies is odd.[23] The same omission often happens in the larger population-level correlation studies mentioned earlier, where an increase in suicides gets closely tied to a decrease in antidepressant use (with any comparable exploration of the impact of discontinuation effects).
Once again, it’s well-known among doctors that one of the most dangerous periods for heightened suicide risk is when dosage changes and tapering happen – with many sorts of adverse effects possible. In addition to significantly less new prescriptions being issued, it’s likely that the black-box warning triggered many dosage changes for youth as well. If so, wouldn’t we expect there to be more frequent reports of uncharacteristic behavior, including suicidality, at least in the immediate, short-term period after the warning? [24]
2. Inacccurate extrapolation. The problems with these studies go deeper than a lack of acknowledging discontinuation effects. In re-analyzing Gibbons’ article, Dr. Mark Stone identifies the way in which an inaccurate extrapolation from the data was made. in particular, he points out how “two time series in separate graphs” have been popularly interpreted: “One showed a steady increase in antidepressant prescribing to U.S. adolescents, with a notable downtick in the last year of the series; the other showed a steady decrease in suicide rates among U.S. adolescents, with a notable uptick at the end. It seemed obvious to many observers that the two were related.”
He continued, “Apparently, none of the authors, reviewers, or editors had noticed that the prescription downtick occurred in 2005, whereas the suicide uptick had occurred in 2004,” adding, “It seemed that people who feared adverse consequences from the boxed warning were poised to believe any allegation that supported their concerns.”[25] (The eagerness to confirm a particular conclusion shows up in the 2014 study as well, in their willingness to use a dubious proxy as a measure for suicide risk).[26]
Dr. Stone notes, “despite the admitted error, the report was never retracted and is still widely cited.”
3. Inaccurate prediction. So adamant was Gibbons’ research team at the greater risk society was placing on children by not providing antidepressants, that they made the following prediction: “In children 5–14 years of age, a 30% reduction in SSRI prescriptions would lead to an estimated increase of 81 suicides per year, or 0.20 suicides per 100,000.”
Contrary to their prediction, however, in the years following that short period surrounding what appeared to be an early spike in suicidal behavior, youth suicide declined consistently every year from 2005 to 2007, reaching a record low that year (4 years after the black box warning), even as the suicide rate for other groups increased.
How much attention has that received?
Very little. It’s definitely not what you hear in media reports about the black box warning.
Instead, virtually all public commentaries about the black box warning hew to the concerns Gibbons, Lu and others have raised. Even when more reliable data emerged confirming and clarifying the picture [27] the “less antidepressants/more suicide” connection is what continues to be shared. Dr. Marc Stone writes with some admitted frustration the way in which those voicing the predominant interpretations “have been undeterred when their favored findings cannot be replicated when better information sources are used. These [additional sources of] data should be sufficient to dispel any serious concerns, but nearly 10 years after the labeling changes, the idea that the boxed warning had adverse consequences persists in the minds of many health professionals, in the media, and among the general public.”
In this way, disproportionate attention continues to be given to some interpretations of the research, compared to others. In the same moment critical details highlighted above are largely ignored, popular (and dubious) conclusions from these studies continue to be circulated widely.
But why? Wouldn’t we be motivated to learn the truth about what’s going to reduce suicide for our youth?
Of course we are. And for that reason, I share Dr. Stone’s distress and disappointment at the degree to which simplistic conclusions are being passed along without critical examination – and the way in which these conclusions continue to be heard, and repeated, and promoted, over and over.
Wide lens vs. narrow lens. One of my own conclusions as to why this is happening, is that people are coming from very different lenses. And if we come at the problem too narrowly, we simply miss the bigger reality of what’s happening. This makes faulty conclusions likely to be shared widely. For instance, we may see an initial positive bump when someone starts an antidepressant, and immediately conclude, “this is surely the answer!” OR we may see some turbulence as someone tapers down, and conclude “your brain can’t work without these!”
In the absence of a wider lens, these conclusions can stick (and with surprising persistence, as I found in my dissertation). That same pattern is what seems to be happening at a broader level. Just as times of discontinuing antidepressants are uniquely turbulent periods for an individual, it shouldn’t surprise us to see a worsening on a collective level during a time when many are being tapered down. And likewise, just as the risk is greater for any individual starting or shifting a dosage, it shouldn’t surprise us to see spikes in harm during periods when more people are starting – or a generic drug comes into the market and people are shifting prescriptions. In all these ways (and times), major shifting in prescription patterns should worsen suicidality in some way.
Once again, none of that is very apparent, however, until we zoom out our focus and consider the broader picture across various time periods. Indeed, with a sufficiently narrow focus, you might just come to resonate with Dr. Gibbons’ summary (the Pharma-supported researcher mentioned earlier): “We’re starting to get a very cohesive story, that the highest risk period for suicide is right before treatment is started, and the risk actually comes down once pharmacotherapy or psychotherapy is started.”
Is that clear enough for you? Only if we’re ignoring what happens next! By zooming out, we start to see all sorts of nuance showing up that we might not otherwise see. For instance, we might notice the way in which some patients may experience an initial boost and relief, followed by a worsening course over time. OR, we may see the way in which patients tapering off antidepressants may experience an initial period of withdrawal turbulence, followed by a decrease in these adverse effects over time (and the ways in which the larger suicide numbers following decreases in antidepressant rates mirror this nuance).
Instead of paying attention to these broader patterns, however (especially across many different time periods), too often one particular time period is seized upon as “definitive proof” for the benefits of increasing antidepressant access for youth – discounting or passing over other periods also worth considering. For instance, compared to the selective focus on certain periods recently, there’s been very little public attention to the data from the 1960s and 1970s where both antidepressant rates and suicide rates rose simultaneously.
Let’s insist on a broader, bigger and longer-term perspective for all these questions. Seriously: don’t our precious kids deserve it? [28]
Of course, we agree on that. Where we disagree is how settled the truth of this matter is, and how urgent and crucial it is to explore some of these disagreements.
To reiterate, I have no doubt we’re all motivated by the well-being of the youth. That’s what motivates a doctor prescribing an antidepressant to a child, and that’s what motivates me raising concern about some potential (inadvertent) consequences of this same decision.
If noble, heart-felt intentions were enough to stop suicide, we’d be in a great place by now. But obviously it’s going to take something far more than good intentions, more “more conversation” or even “more funding” and “more programming.”
I’m convinced that the crucial success we’re seeking will depend on a different kind of conversation – one in which we’re willing to consider (really consider) the possibility of overlooked, inadvertent, unintentional influences from otherwise cherished and trusted interventions.
Are we willing to engage in this kind of a serious, painful exploration, even (and especially) if we don’t like what we see?
Scaling the risk. For those who have taken a careful look at the risk of antidepressant treatment for youth, this question can still remain: How significant is this risk across a population of millions of youth? In the overall “risk-benefit ratio,” could some kind of a risk be worth the benefit of providing help to so many others?
This is precisely what many have concluded. Lu and colleagues write that, “Undertreating depression is worse than the slight increase in suicidal thoughts antidepressants may cause.” And from this vantage point, one doctor described the “2% absolute increase” in suicide risk as “a minor ambiguous effect.”
This raises the question, what does it mean to call the documented increase in risk of youth suicide with antidepressants a “minor effect” or merely a “slight increase”?
Certainly, to some this phrase will mean something like, “not a big deal, all things considered….or a risk well-worth taking, when you look at the bigger picture.”
To others, however, this risk is not “minor” in the least. Though this risk may appear small as a percentage point on a page, it becomes more significant when multiplied out to literally millions of kids in treatment across the nation. As Dr. Healy admits, “It has been difficult to document the relatively rare but very serious risk of suicide,” but adds, “We documented a difference in absolute risk of 5.6 suicide attempts per 1000 patient years of SSRI exposure compared with placebo. Although small, the incremental risk remains a very important population health issue because of the widespread use of SSRIs.”
In this way, compared to those who see this suicidal risk as less significant when considering the broader population (“it’s a very small percentage when you look at the broader population”), there are strong arguments to say that this widespread use makes the risk far more significant than if we were talking about a smaller group of kids taking the drugs. This research team goes on to illustrate that in the United Kingdom alone, “1 million person years of SSRI treatment are provided annually by general practitioners.”[29] If you run the math on that, then that smaller risk they mentioned amounts to 5600 suicide attempts per year across all of the United Kingdom alone, attributed to the added risk of antidepressant treatment.
If we were to assume that the general pediatric antidepressant usage rate in America per capita is roughly equivalent to the United Kingdom, then that would translate into 28,000 youth suicide attempts per year in the United States influenced in some way by antidepressants.
Does that sound like a “minor effect” to you?
What if one of those “minor effects” is your son or daughter? Laying aside the bigger numbers, what if one of your own loved ones is one of the recipients of the “slight increase” that is now widely acknowledged to be a part of the youth antidepressant landscape?
In that case, it’s very difficult to talk about this as a “small” risk, right?
“All treatments have side effects, right?” Nonetheless, when acknowledged in our current mental health conversation, these kinds of cases are portrayed as a percentage so minuscule as to be hardly worth worrying about. And, indeed, in the way our current mental health conversation is set up, it’s often insisted that we must simply accept some kind of a risk if we are to achieve the benefits of antidepressants for everyone else.
Thus, we come back to the classic dilemma: Do we provide life-saving benefit to millions and risk some getting hurt…OR do we step away from both of these?
If that’s the choice, it’s a tough one – maybe even an impossible one. We can hardly imagine a world where that damned if we do/damned if we don’t decision isn’t necessary. Virtually always, it is taken for granted is the almost universal assertion that “all treatments have risks and benefits” – requiring a difficult balancing act of us. Thus Lu and colleagues caution “doctors to weigh the risk of a drug with the risk of not treating or undertreating the condition.”
From this vantage point, we have to be willing to sacrifice some cost and some risk. If that’s true (and if this kind of a compromise is the best we can hope for), then we need to be aware that we’re being asked to accept that some kids (and adults) will likely be driven to greater suicidality by the very efforts we’re making to try and help them.
Is that the best outcome we can achieve? Or are there other approaches to reducing suicide that don’t involve heightening suicide risk simultaneously?
As strange as that sounds, it’s even stranger that we’re not talking seriously enough about the possibility.
But once again, why not? This brings us back to the question that launched this essay: if there’s so much apparent evidence behind this concern, why are we not discussing it more? And why are we not investing more in side-effect-free alternatives?
It’s impossible to adequately answer that question without taking a serious look at perhaps the largest reason this possibility has been minimized in the public eye. You would think that this conversation about risk is profound enough in the way it directly impacts life that we would have careful, honest conversation about it, scientifically-speaking.
That’s simply not the case. As painful as it is to acknowledge, there is clear evidence that the research on suicide has been subtly and significantly influenced by industry funding in a way that substantially skews the results (and the ensuing public/professional conversation) in a certain direction. If you’re not already frustrated yet, then buckle up.
Overestimating + underestimating reality. “Confusion, manipulation, and institutional failure” was how a 2004 Lancet editorial characterized the research into selective serotonin reuptake inhibitor (SSRI) use in childhood depression. The editors’ conclusions were based on revelations that pharmaceutical companies had selectively reported favorable research about the use of antidepressants in children.
The editors write, “That such an event [suicide] could be precipitated by a supposedly beneficial drug is a catastrophe. The idea of that drug’s use being based on selective reporting of favorable research should be unimaginable.”[30]
Dr. Jonathan Leo elaborates, “What seems to bother The Lancet editors, and others, is that, as a body of research, there seems to be a systematic bias toward downplaying the suicide issue.”
Rather than a conscious, malevolent downplaying, I believe that a large proportion of the skew arises in methodological decisions that influence the conclusions in perhaps a largely unconscious way. Looking across studies, there are at least four main ways the research has been “set up” in a way that favors the beneficial effects of antidepressants, while understating the risks:
1. Overly focused on short-term. Consistent with the “wide/narrow lens” discussion above, clinical trials have focused largely on more immediate symptom relief, rather than longer-term outcomes, such as complete resolution of depression, prevention of relapse, and quality of life. According to one review, the mean duration of treatment and follow up in published trials was 10.8 weeks with the vast majority of studies (93% of patients) followed less than three months.
Speaking to the uncertainty that remains without longer-term data, Dr. Newman, a member of the Psychopharmacologic Drugs and Pediatric Advisory Committee that helped review evidence of suicide in youth, said the following:
The FDA’s meta-analysis suggested that the new antidepressants double the risk of suicidality, from about 2.5 percent to 5 percent, in trials lasting two or three months. But what happens if you take them for a year? Does a 5 percent risk over the course of three months become a 20 percent risk over the course of a year, or does the benefit–risk balance improve over time? Does the increase in the rate of suicidality translate into an increase in the rate of completed suicide? Do additional adverse effects occur after treatment with the medications is stopped? Are there important differences among the drugs in this class? What age groups are at risk?
2. Samples too small to detect. If the sample is small enough, it’s more likely you simply won’t pick up on a side effect showing up in a smaller percentage of the population. Most of the trials conducted on children (and adults), however, used smaller samples than would be required to clearly document suicidality. Thus, Dr. Hammad and colleague wrote in the original FDA analysis, “the finding of no completed suicides among the approximately 4600 patients in the 24 trials evaluated does not provide much reassurance regarding a small increase in the risk of suicide because this sample is not large enough to detect such an effect.” And Drs. Gunnel and Ashby likewise shared their concern that “the number of ‘antidepressant induced’ suicides would be small enough to be masked by currently favorable suicide trends.”
In addition to smaller samples overriding effects, there is also evidence that overly heterogenous and broad samples can have the same dilution effect. As Dr. Healy pointed out in 2009, “The 1990s’ data fail to distinguish between the 80% of antidepressants administered in longer-term treatment to patients at little risk from their treatment, and the at-risk group of first-exposure patients who take possibly no more than 20% of antidepressant prescriptions in any 1 year.”
3. Omitting data for various reasons. It’s common for people to argue that no “real suicides” actually happened in the pediatric studies cited above. For instance, Gibbons and colleagues stated in 2007 : “A major limitation of the studies in the FDA’s database is that no suicides were reported in the pediatric studies.”
At a later date, unfortunately, additional data came to light that was not shared forthrightly in the original studies. As Dr. Leo points out, “There is no mention in the [1997 Emslie] paper about any children attempting suicide. However, in the FDA’s ‘Medical Review of Prozac,’ written in 2001 but not made public until 2003, there is a discussion about two children on Prozac attempting suicide.”
Perhaps the most common way these data omissions happen is the “file drawer problem,” wherein studies with unfavorable results are not published. A 2016 Netherlands review notes both “limitations in study design” and “discrepancies in reporting,” as both potentially involved in what they called a “serious underreporting of harms” – reflected, for instance, in “missing data in the summary trial reports on Eli Lilly’s website.”
Sometimes preestablished thresholds are presented as a rationale for not reporting an adverse effect. In one paper by Alderman and his colleagues, the authors decided to only publish side effects that occurred in 10% or more of the patients, which excused them from reporting the fact that 9% of the children on Zoloft in their study had engaged in a suicidal act.” As Dr. Fergusson et al., noted, “One hundred and four of the 702 trials reported adverse events that occurred in excess of a prespecified threshold of either 3%, 5%, or 10% of patients or above a certain number of patients (for example, three patients). As a consequence, rare but lethal complications may have gone unreported or under-reported.”
In other cases, adverse effects are framed in labeled in a way that can feel more palatable and less concerning. As Dr. Leo again notes, one study of Paxil (Protocol 329) included an extensive list of 32 side effects such as nausea, vomiting, chest pain, and so forth. Despite some suspicion at the time that they also led to increased thoughts of suicide, no mention was made of any children having any suicidal thoughts or attempting suicide in the published version of the study. At a later date, at the urging of the British government, GlaxoSmithKline acknowledged that in Protocol 329’s Paxil-treated group, there were 5 children out of 93 who had suicidal thoughts, compared to none of the 89 children in the placebo group with any suicidal thoughts (a finding that had been obscured due to labeling these children as experiencing “emotional lability” in the published study).
Prior to this revelation the average physician would have been left completely ignorant of this vital statistic.
4. Setting up a uniquely unrepresentative comparison. In perhaps the most significant influence over research, there are several ways in which study samples of children become refined over time in ways that affect the results.
Pre-screening. In a variety of ways, it’s common for research teams to eliminate certain people from a study design in advance. Although the intention of doing so is to create a fair comparison, it’s also become clear that some of the eliminations have also led to an especially favorable comparison study. For instance, two of the original Prozac studies on children (and several of the others), included a “placebo washout phase,” which involved putting all the patients on a placebo for a specified time period and then dropping those patients that improved. Dr. Leo summarizes further detail in his 2006 piece: “In the first Prozac study, 10 children were dropped from the study during the placebo washout. In the second Prozac study, there was a run-in phase to preselect for drug responders.” [31] He continued, “All the Prozac-treated children in this study were given 10 mg for the first week, and children who did not respond, or who had negative responses, could then be dropped from the study.” [32] As Dr. Gibbons and colleagues even acknowledge, “the randomized controlled trials analyzed by the FDA systematically excluded patients who were actively suicidal, and thus the FDA lacks data on those who are at highest risk of suicide.”
In addition to this, one of the exclusion criteria for entry into this study was a “history of failure to respond to a clinically adequate dosing regimen of an SSRI.” Dr. Fergusson et al. summarizes, “In 29 trials representing 4243 patients, investigators limited trial entry to those patients who were known to respond to and tolerate SSRIs. Restricting eligibility in this manner would effectively diminish adverse events during the conduct of the trial.” In other words, those who have not responded to prior SSRI treatment were excluded, but it seems that another way to word this would be: “Our study, designed to determine if SSRI treatment successfully treats depression, will only use those children who have been successfully treated with an SSRI for depression.”
High dropout. In addition to advance, deliberate screening of people out, it’s also well-known that many patients drop-out on their own. For instance, in one of the early Zoloft for children studies, Dr. Leo points out that “17 of the Zoloft-treated children, compared to 5 placebo-treated children, dropped out because of serious adverse events.”
How common are these dropouts? In a review of 702 trials, Dr. Fergusson’s team found that out of 493 trials reporting dropout rates (209 did not), 18,217 people (28.7% of the total study sample of 63,478 patients) dropped out. They go on to acknowledge, “ It is well known that patients who drop out tend to have difficulties with treatment and have greater frequency of adverse outcomes compared with other patients in trials.” The authors conclude that “high rates of losses to follow up may therefore have hindered the ability to detect risks of suicide.”
Placebo problems. Given that many participants in these trials have a history of psychiatric treatment, Dr. Healy notes that many in the placebo group were still withdrawing from medications. As Dr. Fergusson again points out, “some trials enrolled patients receiving SSRIs into a placebo arm without an adequate washout period, thereby potentially attributing adverse events associated with the discontinuation of treatment to the placebo or attributing adverse events to placebo in patients who were successfully treated by SSRIs.”
As reflected here, many studies involved an arbitrarily short time frame, an inappropriately small sample size, and an especially unrepresentative comparison – with especially negative events omitted for various reasons. In his own summary Dr. Leo notes, “before the study even started, there was a mechanism in place to maximize any difference between the drug and placebo groups— the placebo group was preselected for nonresponders, while the drug group was preselected for responders. Yet even with this advantage, for the prospectively defined primary outcome measure, 65% of the children on Prozac had a beneficial response compared to 53% of the placebo patients, a result that was not statistically significant. It was only by looking at other measures that clinical significance was found; on the patient- and parent-rated scales there was no advantage to Prozac, but on one of the clinician-rated scales there was a slight advantage to Prozac.”
In all these ways, results of these studies have overstated benefits and downplayed risks. That was the conclusion of a 2004 article by Jon Jureidini and colleagues in the British Medical Journal (BMJ) reviewing SSRI research related to children, where they concluded that the authors of the original papers had exaggerated the benefits and downplayed the risks. Dr. Healy noted in 2009 how “the data from controlled trials indicate that clinicians treating both adults and children appear to overestimate the benefits of treatment, claiming the treatments work when 80% of the response is reproduced by placebo. The data now available call for a judicious skepticism regarding the benefits of treatment and a real concern about hazards.”
Dr. Healy goes on to say that “The studies involving the three most common selective serotonin reuptake inhibitors (SSRIs)—Prozac, Paxil, and Zoloft—serve as excellent examples of how, at every step of the way, the benefits were overestimated and the risks underestimated,” adding, “There is probably no other area of medicine in which the academic literature is so at odds with the raw data.”
Rethinking our ratio: “Benefits outweigh risks”? The practical result of these patterns above is clear: neither patients or doctors were given the whole picture. As Dr. Leo notes, “Doctors trying to weigh the pros and cons of prescribing these drugs were not given all the information in the medical literature; only by reading government reports would doctors have known that, individually, each trial was a failure.”
In the absence of this kind of awareness, both the public and professional conversations have come to be significantly influenced by remarkably absolute statements like these:
- “Paroxetine [Paxil] is generally well tolerated and effective for major depression in adolescents” (2001)[33]
- Zoloft “is an effective and well-tolerated short-term treatment for children and adolescents with Major Depressive Disorder” (2003)[34]
- “There is sufficient evidence to conclude that, overall, SSRIs are effective in treating depression in children and adolescents” (2004)[35]
- “Antidepressants are in fact efficacious in the treatment of childhood depression and that the overall benefit to risk ratio is clearly positive” (2007)[36]
No wonder doctors and parents are not talking about this! Understandably and unsurprisingly, they have put their assurance in research conclusions presented them as true. Speaking empathetically of the conclusions these physicians have reached, Dr. Leo summarizes, “They put their trust in the drugs because they were backed by papers that were: written by professors at the major academic medical centers; approved by peer reviewers; published in the major medical journals; cited in review articles; discussed at meetings; defended by The American College of Neuropsychopharmacology; and, underlying everything, given NIMH’s stamp of approval.”
That’s undoubtedly why physicians, community leaders and parents in my home state of Utah have also done the same. Indeed, in the wake of the suicide spike happening, one prominent physician in Utah has been telling people that “75% of youth who are on SSRIs get better.”[37]
Dear good doctor: What does it mean to “get better”? Are we talking about long-term well-being or some kind of short-term stability (during the time of study measurement)?
If we are to make any significant progress in reducing suicides, we must take a wider lens and insist on the conversation about research and treatment effects free from the subtle (and widespread) distortions of industry influence.
And what happens within this kind of an exploration?
Conclusion from re-analysis of youth data: Risks outweigh benefits. Dr. Newman, who helped advise the FDA on its suicide labeling, concluded as follows: “I found the evidence of efficacy much less convincing than the evidence of harm. In reviewing TADS, we were struck by the small size of the difference between fluoxetine and placebo as compared with the effect of placebo alone. For example, after 12 weeks, the average decrease in the Childhood Depression Scale–Revised (scores on which were around 60 of a possible 113 at baseline in both groups, with higher scores indicating more severe depression) was 19.4 points with placebo, as compared with 22.6 points with fluoxetine.”
Dr. Newman added, “It is easy to see why the personal experience of clinicians and patients would lead them to believe the drug to be effective, since they would have no way of knowing that more than 85 percent of the benefit they observed would also have occurred with placebo. Randomized trials other than TADS have had less favorable results. The FDA indicated that only 3 of 15 trials of antidepressant use in children with depression had found a statistically significant benefit. The agency also provided us with a meta-analysis that showed that the estimated efficacy of antidepressants in children was minimal and likely to have been overestimated, because published studies have much more favorable results than unpublished studies. Thus, both clinical experience and published trials are likely to lead to inflated estimates of the efficacy of these drugs.”
In 2004, Dr. Whittington from University College, London compared research findings that had been published, with findings unpublished: “Published results from one trial of paroxetine and two trials of sertraline suggest equivocal or weak positive risk-benefit profiles. However, in both cases, addition of unpublished data indicates that risks outweigh benefits.” Thus, once the unpublished literature is included in the risk-benefit analysis of these drugs, the benefits do not outweigh the risks. Listen to their conclusion, summarized in another way: “Published data suggest a favourable risk-benefit profile for some SSRIs; however, addition of unpublished data indicates that risks could outweigh benefits of these drugs (except fluoxetine) to treat depression in children and young people.”
This is similar to others’ conclusions. As reported by Dr. Leo, “One of the investigators involved with the Zoloft study, who was not an author and, apparently, not privy to drafts of the paper, eventually wrote a letter to JAMA after the study was published, pointing out some of the very concerns that the reviewers should have spotted. Though the letter unfortunately went unpublished, it stated that the conclusions of the paper should have been: “Sertraline is ineffective when compared to placebo and is associated with increased adverse events.”[38]
This may be the case with one trial. But it’s important to know how frequent such disappointing results show up?
As Goodman noted in 2006, only 3 of the 15 trials submitted to the FDA demonstrated superiority of the drug effect over placebo. “Besides concerns about suicide, there is a very good reason for not taking the drugs: They simply don’t work very well.” They note “Even in the adult studies, the difference between the percentages of favorable responses in the drug-treated group compared to favorable responses in the placebo group is minimal” (citing Kirsch, Moore, Scoboria, & Nicholls, 2002). Dr. Healy similarly state, “According to the data, the efficacy of Prozac is not very significant. Using the researchers’ own criteria for defining an ‘improvement,’ and taking into account the large placebo effect, for every ten children it is given to, it maybe helps one patient.”
In these other risk-benefit analyses, given such little benefit, there seems to be little justification for putting up with the identified suicide risk. And indeed, whatever disagreements others may have, Dr. Leo points out that this data was “incriminating enough to convince two governments to intercede; the Americans with a warning label, and the British with an outright ban on several of the medications for people under 18 years of age.”
Note to physicians: This is NOT an “anti-med” or “anti-doctor” message. As medical journalist Bob Whitaker articulated in my interview with him, there’s obviously a crucial and important place for doctors in this ongoing conversation. Rather, this is about critically examining best practice, with a careful focus on possible iatrogenic effects in line with the foundational Hippocratic oath to Do No Harm.
Changing our conversation on youth suicide. What are the consequences of all the above data?
First, we need to stop believing the popular idea that as long as these kids are getting treatment they’ll be safer.
That’s simply not true. It all depends on what kind of treatment, how long, etc.
In other words, more access to services, broadly speaking, may or may not be moving our suicide numbers in a better direction.
Secondly, at the very least, let’s make space in our public and professional conversations for a robust exploration of the established risks of anti-depressant use for children and adolescents. That would be the scientifically honest and professionally ethical thing to do.
Are these conclusions a “little extreme”? I’m well aware how raising these concerns with those unfamiliar with this data can make you sound just plain crazy … especially because most parents, most legislators, most counselors, and most doctors have never explored this issue in great depth (some definitely have).
But from the vantage point of the established research, should we really be surprised? If clinical studies consistently show a doubling of risk for suicidal behavior in adolescents, and if these treatments have doubled or tripled in Utah in the last decade, would we not expect suicidal outcomes to increase in Utah (or anywhere else where massive expansion of antidepressant treatment rates among youth are seen)?
If nothing else, however, I hope this review makes clear how crazy it feels to those of us familiar with this research literature to hear people calling for more children and adolescents on antidepressants.
Haven’t we tried that experiment already? And aren’t things worse than ever before?
Rather than repeat the same decades’ old arguments about under-treatment, could it not be a good time to rethink the whole approach?
I’m convinced it’s time to have a more direct public discourse about these questions together, exploring questions such as these:
- Are our families better off than we were before our youth started on antidepressants?
- Are our children currently medicated with antidepressants doing well (really well?)
- Are children facing depression who are not medicated doing comparatively worse over time?
- Are we finding any other ways to support youth facing depression that do not involve any such risk to worsen suicide?
Don’t ignore this. Please don’t.
For all the many reasons reviewed above, I believe these concerns have merit. I only hope that more of us can see this sooner rather than later. If we do not change course, and specifically, if we increase the number of our youth on antidepressants (especially long-term), I believe that suicides will continue to increase.
If that’s what happens, then in the spring of 2019, I fear we will be talking about why the suicides have gotten even worse in Utah (and elsewhere).
Let’s make sure that doesn’t happen.
Appendix: Five additional points.
1. Far bigger than meds. So wait, haven’t I just argued about one factor responsible for an increase in suicides? Yes, I have argued that this single factor could be having a disproportionate influence on the rising rates. As stated initially, however, I stick by the reality that suicide is always complex. Even those whose suicides are determined to be drug-induced have many other factors in their lives that contributed to that outcome. I believe that is the case always.
Clearly, the conversation needs to focus on far more than just the medications. I write about them here because they’re receiving so little comparable attention. People took their lives long before antidepressants were in the picture, and they do so in most cases without any influence from them. That’s why I’ve also written about the kinds of messages that might prompt a sense of learned hopelessness.[39]
2. Risk-factor free alternatives. In terms of public health interventions, could there possibly be another way that doesn’t require a risk and lose so much for the “good of the whole”? But, of course, there is. And, of course, there are hundreds of things that can help increase people’s desire to live without (in the same moment) exacerbating the risk of people killing themselves.
What if we were to invest and emphasize and focus on those as our first line interventions to address suicide? Imagine a mass suicide prevention effort centered on interventions for our youth without any chance of raising the suicide risk?
I personally believe this kind of an initiative would be much more in line with the expansive, wide-ranging, spirit-oriented message (mentioned earlier) that Elder Jeffrey R. Holland shared with Latter-day Saints about mental health.
In line with this, I’m launching my own development/research project this summer and am searching for seven research assistants to assist. To participate, you need to be able to contribute 5-10 hours/week and have a passion for this topic. Students, working adults, or retirees are all welcome. You can work out of home. And I will train you. Send me a note on the contact form of this website if you have interest in hearing more! If you have any interest in financially supporting that research project, I’d welcome your inquiry.
3. Different levels of awareness. I want to underscore that the kinds of interpretive issues explored above are simply not something most professionals (or researchers) are even aware of, in my experience. Indeed, the lack of awareness runs deep – as illustrated in one review of 702 clinical trials of antidepressants, where remarkably “only one trial mentioned a potential association between suicidality or any aspect of self-inflicted injuries and SSRIs in their background or discussion sections despite repeated concerns about this adverse effect expressed in scientific discourse.”
That being said, we would be foolish not to acknowledge that there are people who have been aware of the discrepancies. As has been extensively documented elsewhere, some people within different companies have been aware of the manipulations. How exactly to respond to these patterns, and hold industry accountability is a question for others to resolve. It is hard, however, not to note the similar patterns that have led to a growing number of lawsuits targeting industry marketing practices that contributed directly (and indirectly) to the opioid epidemic in America.
4. Changing the way we do things. There are many possible adjustments that may arise from greater awareness of these patterns. For instance, Leslie called in 2005 for the following: “Push for disclosure to the public of all safety and efficacy results found in drug trials, including those that do not support the hypothesis being tested or that are contrary to the intended outcome.”
It was mentioned earlier that additional physician training will be happening in Utah, in hopes it will “decrease Utah’s suicide rate by at least 10 percent by 2021.” That involves, “training to providers and access to treatment for teens who need it.”
What would it mean for this physician training to take this research seriously? I close with some summary recommendations for physicians gathered from different articles in this review.
Recommendations:
- Encourage families to explore other options prior to initiating antidepressant treatment. Dr Timothy Spruill “despite the fact that the Cochrane review of the evidence confirms the effectiveness of counseling for depressed patients, why is it that consumer use and physician referral for counseling continues to decline.” Alongside management of symptoms, it’s important to bring more intervention focus to root contributors. Dr. Tomi Gomory, a professor of social work at Florida State University, told me, “A focus on chemicals can become a way of avoiding the harder conversations about changes needed in the social environment. Why are young people in such existential crisis?” He went on to talk about “enormous existential pressure placed on kids” in society today – pointing out that “treatment does not actually focus on why children end up killing themselves.”
- Don’t ignore the black box warning for youth. Contrary to the popular dismissals and warnings about the suicide risk, it’s time to stop ignoring the clear risk for some youth and adolescents on the antidepressants.
- Reconsider the risk/benefit profile. As noted above, it’s also time to have a more serious conversation about the true risk/benefit profile of antidepressants for youth, removing the distorting influence of industry.
- More robust informed consent. Dr. Newman, a member of the Psychopharmacologic Drugs and Pediatric Advisory Committee that helped review evidence of suicide in youth, said this “this controversy over the use of antidepressants in children illustrates the need for a more sophisticated approach to evaluating harms and efficacy than simply seeing whether they are statistically significant at a P value of less than 0.05. Regardless of the P value, no psychotropic drug is free of potential negative effects. The best available estimates of the magnitude and nature of the effects of the drugs must be discussed with patients and families, so that they can make an informed decision about treatment.” Speaking of informed consent, Dr. Tomi Gomory told me in personal correspondence, “we need a fully transparent discussion of the pro’s and cons. Providers rarely, if ever, identity all the adverse effects and reactions.”
- Closer monitoring, especially of children and adolescents. The most common recommendation to emerge from all the studies I’ve reviewed was a consistent plea for physicians (and parents) to watch more carefully signs of worsening. This comes up over and over and over in the research articles: Dr. Leslie and colleagues call for “generally at least weekly contact during the first 4 weeks, with specific visit intervals specified after those 4 weeks.” Shauna Reinblatt and colleagues call for “Close monitoring for [adverse effects], not only when initiating SSRI treatment but also throughout dose titration,” as a recommendation “for early identification of activation.” To reiterate an earlier important mention, Dr. Jane Garland and colleagues warn for careful monitoring of children, especially given the many ways we might miss them, including “(a) the similarity of some adverse effects to depression’s own symptoms, (b) a child’s lack of insight in recognizing them this and (c) the fact that the onset of this lack of motivation comes later on in treatment.” Christiansen and colleagues recommend “systematic risk assessment in the period after redeeming the first prescription.” Dr. Olfson states that “These findings support careful clinical monitoring during antidepressant drug treatment of severely depressed young people.” And Umetsu and colleagues add, “Children and adolescents should be closely monitored for the occurrence of suicidality when they are prescribed SSRIs.”
- More support for gradual, carefully tapered reductions. Help patients taper off if and when they feel ready. In many cases where tapering happens, however, physicians have received little training on safe and effective discontinuation. For those doctors seeking an expanded skill-set, there was a great training that happened in 2017 (recorded and available here) – and another in 2018. Luckily, there is also a growing amount of powerful information to guide individual patients and families on the gradual, personalized, careful, and managed tapering process people need to be successful (slow and mindful enough to manage withdrawal effects). This ideally should be done with professional oversight. Check out Laura Delano’s Withdrawal Project as a great place to find more guidance.
- Stop telling patients they need to be on antidepressants life-long. This is happening a lot, with patients experiencing various mental/emotional conditions – including with children. Please stop telling people this, and help them appreciate the possibility of tapering off one day if-and-when the time is right (and with appropriate supervision). As I’ve written and spoken about extensively, the life-long treatment message can be, for some, such a despairing message for people to hear – and undoubtedly, has contributed to some people reaching a place of lethal despair (see these essays, these videos + this class).
5. Reiterating the spirit of my analysis. To reiterate, losing one life (of any age) to suicide is one too much. We all know that. And so, we’re doing ALL we can to stop it – in Utah and across the nation. In addition to all the new programs, grants and funding, I wonder: Are we willing to have especially difficult conversations that might make a significant difference in reducing these numbers?
In the above essay, I have reviewed the surprisingly robust evidence for a contributing factor that’s rarely discussed in our conversation about youth suicide. I believe that’s a tragic oversight – and I’ve done my best to show you why. One reason (among many I review) that we don’t raise concern about this factor is we’re so busy promoting it as one of THE primary answers to reducing suicide among our youth – with ongoing, consistent messaging still often being shared about the danger of “under-treatment” in our youth. In response to that viewpoint, I’ve shared the above information deserving, I believe, of urgent public health consideration.
That being said, I’ve presented this as one perspective in a conversation with many different views, taking for granted that we’re all doing our best based on what we know, and that we are united by a shared desire to find better solutions. I encourage all individuals and families currently facing mental distress to continue working with anyone helping you navigate these important questions, including professional support, and to work carefully on a plan that you and your family feel the most peace about pursuing.
Citations:
[1] Despite all the valiant efforts to reduce suicide rates in the U.S., a study by the National Center for Health Statistics released in April of 2016 reported that suicide in the United States had surged to the highest levels in nearly 30 years, with an increase in every age group except older adults. The rise was especially pronounced in middle-aged women (up 63%) and middle-aged men (up 43%), with the overall suicide rate rising by 24 percent from 1999 to 2014.
[2] These are questions deserving of careful inquiry and gentle care, as well as space for thoughtful and honest disagreement. Unfortunately, this conversation has more often become the site for emotionally-charged attacks and accusations that help no one – certainly not the teens we are all trying to help. These concerns have prompted some of my writing and speaking on the topic in recent years:
- Yes, Let’s PLEASE Have a Serious Conversation About Suicide! Questions for the Public Conversation
- Can we stop pretending there is only ONE reasonable explanation for the tragic suicides of LGBT-identifying religious youth?
- Why I Believe the Mama Dragon Approach Is Ultimately Hurting Teens & Families (Despite Earnest Intentions Otherwise)
- A Plea for a More Honest + Less Despairing LBGT-Religious Conservative Conversation
[3] Let me be clear about three things: NO one is a bigger Elder Holland fan than me. If they sold Apostle T-shirts, I’d be repping Elder Holland’s! If Church distribution released Apostle action figures, Elder Holland would battle alongside Captain America in my boys’ toy room. So, in other words, I trust and love this man. And I can’t imagine him approving of the way one small part of his talk has been taken and interpreted by some. Furthermore, if my essential argument here is true, I can’t imagine that Elder Holland wouldn’t also be horrified (and be very much interested in talking about this).
[4] But have the treatment rates really increased? I’ve done everything I can to track down this information, but have been unable to find it. Undoubtedly, someone has this information at their fingertips. But as Michael Friedrichs (one of the main Utah state statisticians working on data analysis of this question) told me, we have no way of knowing whether there has been an increase in treatment usage for sure. Admitting to some frustration on his part at the lack of transparency, Michael said that unlike other Western countries, that information is not publicly available from pharmacies. If someone has access to that data, please consider sharing it.
[5] This research team went on to say that “side effects, as a reason for discontinuation, were minimal” (Emslie et al., 1997, p. 1033).
[6] Healy D, Whitaker CJ (2003). “Antidepressants and suicide; Risk-Benefit Conundrums”. J Psychiatry & Neuroscience. 28 (5): 331–339., with response by Y Lapierre 340–349.
[7] It’s also unfortunate that later corporate memos revealed by Eli Lilly confirm a cozy relationship between some of these FDA officials and the industry, with Leber called “our defender” and a note that confirmed, “Lilly and FDA are working together on the suicide issue.”
[8] Allison Bass, “Side Effects: A Prosecutor, a Whistleblower, and a Bestselling Antidepressant on Trial,” Workman Publishing, York, p. 38.
[9] From that same report: “23% of women in their 40s and 50s take antidepressants, a higher percentage than any other group (by age or sex). Women are 2½ times more likely to be taking an antidepressant than men.”
[10] The new data comes from an analysis of the 2013 Medical Expenditure Panel Survey (MEPS), which gathered information on the cost and use of health care in the United States. Moore and Mattison found that nearly 17 percent of adults in the U.S. reported filling at least one prescription for a psychiatric drug in 2013.
[11] In addition, 8.3 percent of adults were prescribed drugs from a group that included sedatives, hypnotics and anti-anxiety drugs, and 1.6 percent of adults were given antipsychotics, the researchers found.
[12] This is true since at least 2005, (see “Astounding increase in antidepressant use by Americans,” OCTOBER 20, 2011, Peter Wehrwein, Contributor, Harvard Health)
[13] “It has been suggested that SSRI usage cannot induce suicides in line with the rates of excess suicides found in randomized controlled trails and other studies because the continuing growth of scripts issued has been accompanied at least in some instances by a fall in suicide rates” (Reseland, et al, 2008, p. 80).
[14] Some of the limitations are summarized below:
- Regression to the mean. “These uncontrolled studies may demonstrate little more than the fact that patients with any condition, from influenza to depression, seek or receive treatment when at their worst, and the natural history of these disorders leads to an improvement in the post-consultation period, even if no effective treatments are available” (Healy, 2009).
- Suicide decrease for other reasons. Reseland et al., note that in Norway, “suicide rates were falling prior to any increase in SSRI consumption, and any effort to explain what is happening must take this point into account.” One 2004 article notes a drop in substance use between 1980 and 2003 as another possible contributor to the decrease in U.S. child and adolescent suicide rates during this period. Marc Stone writes, “Ecological studies that examine geographic variability in antidepressant use often show an inverse relationship with suicide rates, but I believe that these results can best be explained by confounding. The same socioeconomic factors that promote greater availability and use of many prescription drugs (including antidepressants) also lower suicide rates among even the substantial majority of the population that does not take antidepressants.”
- Variation in how suicide is counted. Some have argued that increasing numbers may be a reflection of countries counting suicide more accurately, while others have pointed out that a rapid decline in the use of autopsy across the world may have the reverse effect, leading to a greater likelihood of death by suicide being missed as an ill-defined category.
- Clustering very different kinds of patients. Certain periods of data (such as the 1990’s) “fail to distinguish between the 80% of antidepressants administered in longer-term treatment to patients at little risk from their treatment, and the at-risk group of first-exposure patients who take possibly no more than 20% of antidepressant prescriptions in any 1 year.” As one research team points out, “Once such distinctions are made, it is possible to reconcile an increased exposure to a treatment-induced risk with falling national suicide rates” (Healy, 2009)
[15] For instance (credit to Bob Whitaker):
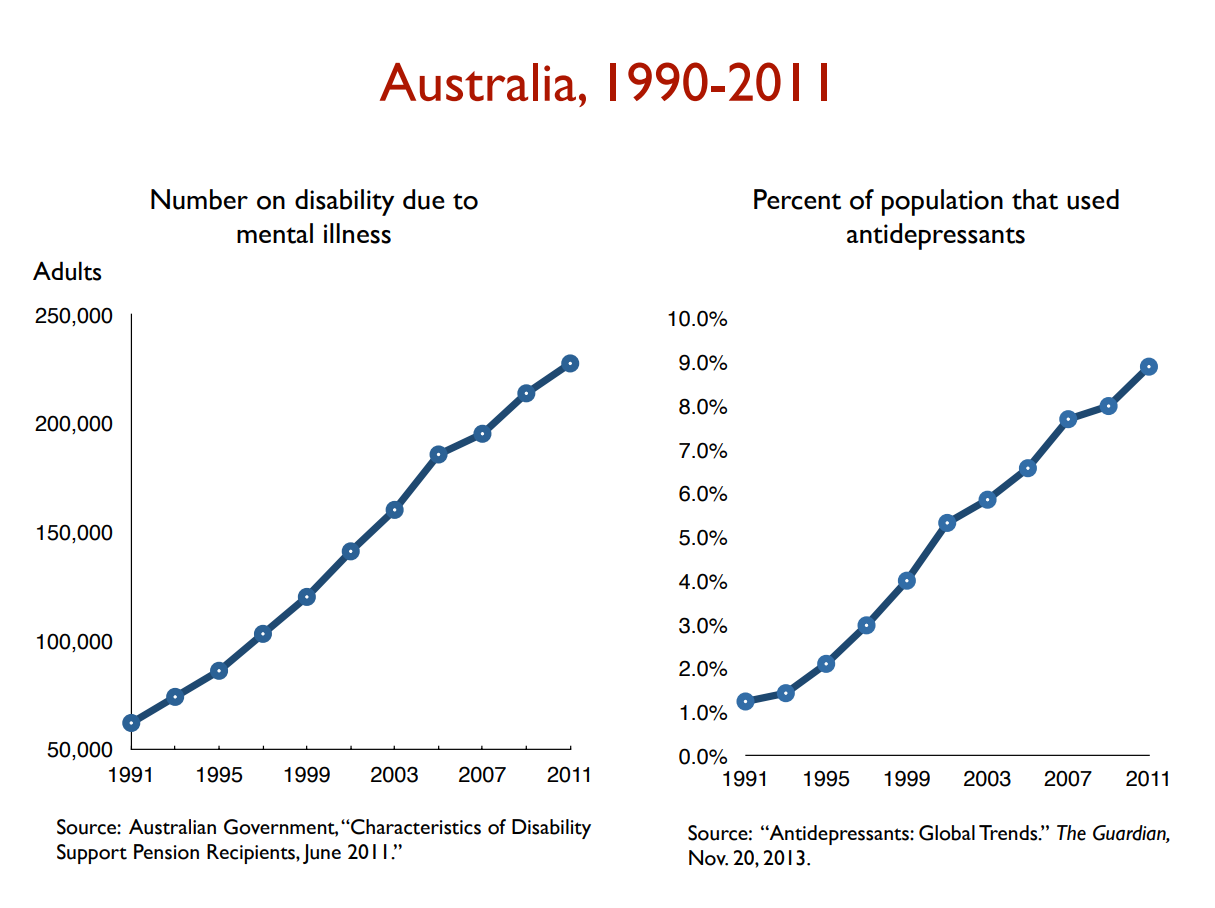
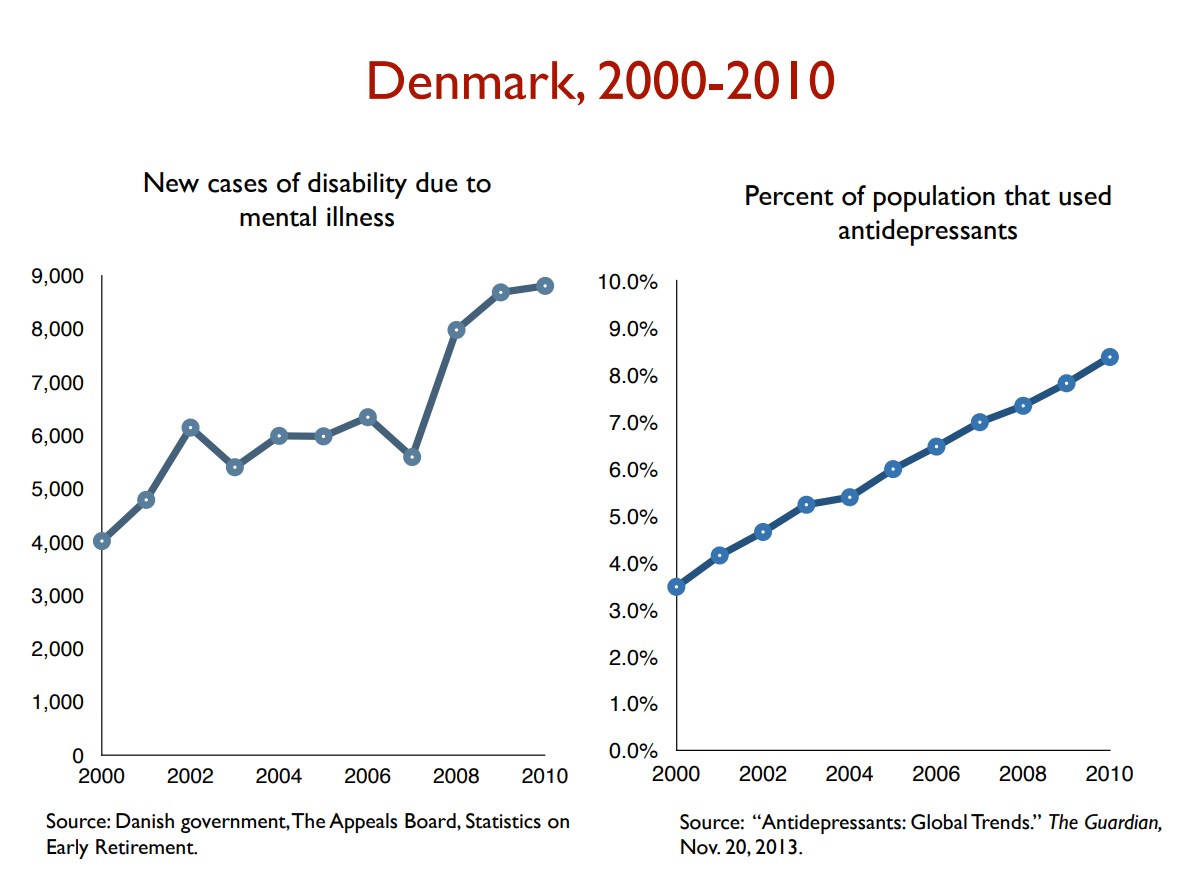


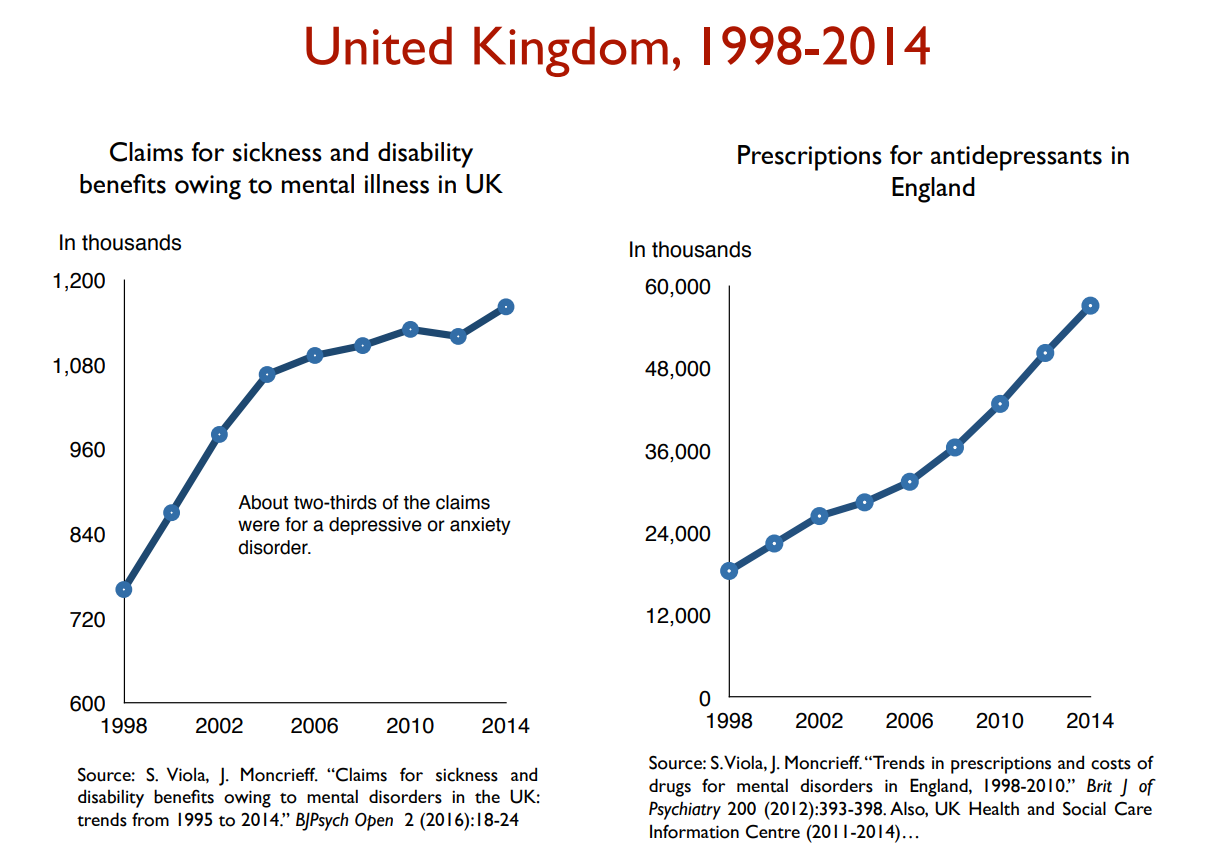

[16] The primary outcome, which was labeled “suicidal behavior or ideation,” contained three elements: Suicide attempts, and/or Preparatory actions towards imminent suicidal behavior, and/or Suicidal ideation. The overall risk ratio (drug vs. placebo) for the three elements combined was found to be 1.95 (95% CI, 1.28 – 2.98). The risk ratio for suicidal behavior (first two items) was 1.90 (95% VCI, 1.00 – 3.63).
[17] (Emphasis added). See also Breggin 2003 and Newman 2004 for additional analyses of the data available at that time.
[18] Expert Working Group on the Safety of Selective Serotonin Reuptake Antidepressants 2004. Safety of antidepressants [Internet]. London (GB): Medical and Healthcare Products Regulatory Agency; 2004 [cited 2006 May 13]. Available from: http://www.mhra.gov.uk/home/ idcplg?IdcService=GET_FILE&dID=1391&noSaveAs=1&Rendition=WEB. 12.

GlaxoSmithKline. Paroxetine adult suidality analysis [Internet]. GlaxoSmithKline; 2006 [updated 2006 Apr 5; cited 2007 Aug 8]. Available from: http://www.gsk.com/media/paroxetine/briefing_doc.pdf.
Stone M, Jones L. Clinical review: relationship between antidepressant drugs and adult suicidality [Internet]. Washington (DC): United States Food and Drug Administration; 2006 [cited 2006 Dec 10]. Table 16, p 26; Table 18, p 30. Available from: http://www.fda.gov/ohrms/dockets/ac/06/briefing/ 2006–4272b1-index.htm.

[credit for both tables to Healy, 2009]
[19] Healy D, Whitaker CJ. (2003) Antidepressants and suicide; Risk-Benefit Conundrums. J Psychiatry & Neuroscience 28 (5) 331-339.
Could they both be true, perhaps – at least, to some degree? (with some patients having lower risk on on antidepressants, and others having their risk raised?) Of course.
While some kind of a compromise between the two positions would seem reasonable and sensible, it is the practical (fiscal and personal) consequences of specific policies that perhaps prevents more of a middle ground approach.
[20] Olfson M, Marcus SC, Shaffer D. Antidepressant Drug Therapy and Suicide in Severely Depressed Children and Adults. Archives of General Psychiatry. 2006 Aug. 63:865-72 .
Two years later, Dr. Olfson and colleagues again found confirmation of this trend with additional analyses.
[21] Here are studies exploring the same phenomenon in adults, in chronological order (from 1990 to 2016): Marin 1990, Diagnosis of apathy; Goldsmith 2001; Barnhart 2004, SSRI apathy syndrome; Reinblatt 2006, SSRI-induced apathy; Wongpakaran 2007, SSRI-induced apathy in elderly.; Moret 2009, Apathy, lack of motivation, frontal lobe syndrome; Sansone 2010, Apathy and indifference; ; El Mallak 2011, chronic depression dysphoria caused by antidepressants; Makris 2012; Perroud 2012; Read 2014, Antidepressant-induced apathy and indifference; Cartright 2016, long term deterioration [Credit – Peter Breggin]
Related to this, one colleague, Al Galves, who has spent years working with people facing these challenges, reminded me about a piece in Peter Kramer’s book Listening to Prozac, where he observed some patients on Prozac having “lost their conscience.” They just didn’t care as much. He continued:
I also have read that most of the psychotropic drugs cause emotional blunting, an impairing of the ability to process emotions. That stuck me because, when a patient of mine tells me s/he is thinking out killing herself or himself, I ask what the advantage of that would be. They pretty much all say something like “It would be all over. I wouldn’t have to deal with this stuff anymore. The pain would be gone.” Then I ask them what would be the disadvantage of it. Everyone says it would be devastating for their friends and family. If you take away that concern and caring you are increasing the risk of suicide.
[22] As Gibbons and colleagues conclude, “Our findings raise concerns about the potential for harm that may result from a decreased use of SSRIs in the pediatric population….the intent of the pediatric black box warning was to save lives, the warning failed, and in fact it may have had the opposite effect; more children and adolescents have committed suicide since it was introduced.”
[23] These researchers portray these concerns in an oversimplified fashion, as if critics believe problems will magically improve once antidepressant use declines – aka, “we would assume that if SSRIs caused suicide, a decrease in SSRI use would lead to a decrease in suicide—and the evidence generated in this study is not consistent with the causal assertion that SSRIs lead to suicide.” They say another time in the article, “If the FDA’s conclusion that there may be a causal link between suicide and antidepressants (which was the basis for the black box warning) were correct, we would have expected to see decreases in the suicide rate during the period of declining SSRI prescription rates, but instead we saw an increase in suicide rates.”
In fact, this is not what theorized, since critics are well-aware of the acute risk that follows discontinuation.
[24] Consistently, Utah’s own Dr. Doug Gray found that discontinuing medications was a common them among youth who die by suicide.
[25] To their credit, this research team admits that they have been professionally supported by five different pharmaceutical companies in various ways.
[26] In Lu and colleagues’ study from 2014, a great deal of attention was given to a presumed increase in “suicide attempts” as measured by a proxy variable called “psychotropic drug poisonings.” While admitting that “completed suicides did not change for any age group,” this increase in “poisoning by psychotropic agents” became the main evidence for heightened suicidality, despite the fact that there was no way they were able to assess motives, intentions or circumstances behind what got labeled as a kind of toxic antidepressant dosage.
Superior data are available from the Centers for Disease Control and Prevention, which prospectively collects data on poisonings and trauma from a statistically valid sample of the entire United States, with on-site determination of the presence of suicidal intent. Like completed suicides, incidents of nonfatal, intentional self-harm (attempted suicide), both from poisonings and from all causes, peaked in 2003 or 2004 and then decreased. The rate of accidental drug poisoning (such as overdoses of drugs of abuse) increased significantly in 2005 and 2006 [see graph provided above – or in his published piece]. Other data sources that provide more direct and valid measures of suicidal behavior among young people (including the Youth Risk Behavior Survey) also show no increase in suicide attempts in this population subsequent to the issuing of the boxed warning.
[28] The contrast between conclusions reached depending on whether your scope of evaluation is short-term or long-term has been a focus of my work in years past (see here and here) – and shows up over and over in the broader conversations about mental health.
[29] North of England Evidence Based Guideline Development Project. Evidence based clinical practice guideline: the choice of anti-depressants for depression in primary care. Report 91. Newcastle upon Tyne: Centre for Health Services Research, 1998.
[30] Editors. (2004). Depressing research. The Lancet, 363, p. 1335
[31] Dubitsky, C. (2004). Review and evaluation of clinical data placebo-controlled antidepressant studies in pediatric
patients. Food and Drug Administration. Retrieved July 2005 from http://www.fda.gov/
ohrms/dockets/ac/04/briefing/2004-4065b1-08-TAB06-Dubitsky-Review.pdf
Emslie, G. J., Heiligenstein, J., Wagner, K. D., Hoog, S. L., Ernest, B. A., Brown, E., et al. (2002).
Fluoxetine for acute treatment of depression in children and adolescents: A placebo-controlled,
randomized clinical trial. Journal of American Academy of Child and Adolescent Psychiatry, 41,
1205–1215.
[32] This is a quote from Dr. Leo (2006) who is citing page 1206 of this study:
Emslie, G. J., Heiligenstein, J., Wagner, K. D., Hoog, S. L., Ernest, B. A., Brown, E., et al. (2002).
Fluoxetine for acute treatment of depression in children and adolescents: A placebo-controlled,
randomized clinical trial. Journal of American Academy of Child and Adolescent Psychiatry, 41,
1205–1215
[33] Keller, M. B., Ryan, N. D., Strober, M., Klein, R., Kutcher, S. P., Birmaher, B., et al. (2001). Efficacy
of paroxetine in the treatment of adolescent major depression: A randomized, controlled
trial. Journal of American Academy of Child and Adolescent Psychiatry, 40, p. 762.
[34] Wagner, K. D., Ambrosini, P., Rynn, M., Wohleberg, C., Greenbaum, M. S., Childress, A., et al.
(2003). Efficacy of sertraline in the treatment of children and adolescents with major depressive
disorder: Two randomized controlled trials. Journal of the American Medical Association, 290,
p. 1033
[35] American College of Neuropsychopharmacology. (2004). Executive summary: Preliminary report of
the task force on SSRIs and suicidal behavior in youth. Available at www.acnp.org/exec_summary.pdf, p. 4.
[36] Gibbons, R.D., et al., (2007) Early Evidence on the Effects of Regulators’ Suicidality Warnings on SSRI Prescriptions and Suicide in Children and Adolescents. The American Journal of Psychiatry, 164(9), pp. 1356-1363
[37] No doubt, referencing a paper written by Dr. Doug Gray concluding that three-quarters of youth who stayed in treatment became less suicidal over time.
[38] Garland, J. (2004). Letter to editor. Unpublished manuscript. Retrieved July 2005 from http://www.ahrp .org/infomail/04/01/09.php
[39] My most developed thinking on “learned hopelessness” is contained in this video, this video, and this longer essay





Please send me more info about helping with this project.
Thank you. It’s so well argued and documented – yet the humanity shines through. Balanced and brilliant.
Thank you.
thank you, Mario!
As a Jr. High School Counselor, youth suicide touches my life deeply. I can think of 5 youth suicide completions just in my small area in the last year that were on medication. I’ve also had a few students with depression study the natural route to healing, and I have seen them improve and grow more resilient. I hope people will look at this discussion seriously.